Responding to lockdown: colleagues from Belfast Health and Social Care Trust share their journey and reflections on service change, outcome monitoring, and future outlook
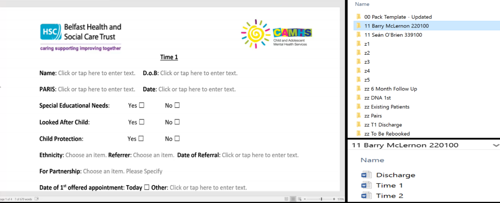
CORC members have told us they are keen to hear how colleagues in other services and areas are adapting to the impact of the coronavirus. As part of a new series sharing members’ experiences and challenges, we sat down (virtually) with CAMHS Outcomes Information Officers Barry McLernon and Seán O’Brien from Belfast Health and Social Care Trust to hear about changes in their service, and to learn more about how they are capturing feedback on outcome and experience as they transition to remote work with children, young people and families.
CORC: How did your service adjust since the lockdown? What’s changed in the service over lockdown?
Sean: Our CAMHS teams are doing lots of initial assessments as capacity has increased slightly due to the sessions being now delivered via phone and/or vide. I was talking to one of the Team Managers and she mentioned that the young people suffering from ASD, for example, were very pleased with not having to come out of their rooms/houses but still “attend” their session via video/phone.
We are also still offering the option of face to face for those emergency cases, but these are scrutinised by team leads to see if it is necessary in the first instance.
In terms of adjusting and in my role as Outcomes Information Officer, is actually realising that we are still at work, but understanding that the returns of outcomes/feedback and the extra work that goes into it should not put extra pressure on people already adjusting to many other new things.
Barry: We are making the most of it and because you don’t see people continuously and are not picking up smaller tasks here and there anymore, you start thinking about more long-term strategic work and projects.
Belfast and South Eastern Trust CAMHS
The service aims to promote emotional wellbeing and deliver care, treatment and preventative mental health services to Belfast’s young people aged up to 18 who experience significant mental health difficulties. The service employs specialist, multi-disciplinary mental health workers who work alongside young people with complex mental health needs and who provide systemic support for parents and carers. CAMHS also offers support and training to staff in schools, youth workers, GPs and others who work alongside young people to raise awareness and ensure timely and appropriate referrals are made.
CORC: What kind of measures are you working with? How easy/difficult is it to work with these measures remotely?
Sean: Well, first, when the lockdown began, we contacted our senior management and said “right, what’s happening? Are we being re-deployed? Is our work as Outcomes Information Officer classified as non-essential? And they said: “No, as far as we are concerned, business as usual as much as you can.” So, with regards to our outcomes we are still asking our teams to complete our digital packs, so collecting demographic info, presenting need, planned intervention, CGAS and GOALS. The SDQ is not being collected for now as no face to face sessions are taking place. We are planning to review this, but this is all dependant on the guidance we receive from our service managers on how long these measures are going to be in place.
CORC: Are you interested in how your service users’ mental health needs link to the Covid-19 pandemic? Are you planning to measure this?
Barry: We added in “Covid Specific Health Anxiety” into the Presenting Problems section of our pack that we send out with clinicians to pick up demographic information. It is to measure how many young people are coming in that are experiencing significant anxiety because of the virus. Nothing as in depth as a metric I am afraid.
We are hoping we can start picking this up in our initial assessments. If we can get the clinicians advising us that the young people are showing Covid-19 related health anxiety and if we can see a trend and notice patterns.
Sean: However, as soon as people can come out of lockdown and start getting to see their GPs again and referrals are made –it might not necessarily be directly linked to Covid-19 anymore, but linked to the impact it had on their families and people losing their jobs and people losing family members and so on.
Barry: It is about what impact this is having on people’s lives economically, socially and on everybody’s mental health and wallets, including systemic issues. Going forward, if we are able to pick up something that is Covid-specific, we are quite pleased. But it will be very difficult. Everybody has a different attitude to it. I for example have no more commuting to do and save £200 a month, but other people lost their job and don’t know how to pay their mortgage.
So, our job is to try and plan for ‘the next time’ so to speak. Doing as much research as possible collectively, so that we might be able to put our services in a better state before another crisis like this, hits us again.
CORC: Which brings me to our next question, how is your service preparing for the period after lockdown?
Sean: Our teams are expecting a surge in referrals once people feel safer to go back to GPs. From my experience in CAMHS, whenever we have seen increases in cases, what we have tended to do is look at triage plans. Triage is basically the assessment to allocate patients to the different teams. In Northern Ireland they have 5 steps. Our triage process is to see if the referral is appropriate for CAMHS. If so, it is then transferred within our system to the appropriate team. If it feels inappropriate, it is either signposted to the most appropriate service or back to the referrer with recommendations.
Barry: Also, our managers are holding a meeting every Monday and are continuously reviewing the situation. We have several team leads asking for referral stats from our crisis teams and we are continuously monitoring that. There will certainly be a backlog. Everybody knows this is going to affect service providers and users on multiple levels. So, we really need to start clearing our waiting lists while we can and be ready for the time after lockdown.
CORC: Are you collecting data about how remote session delivery is being perceived by service users? Might you continue offering video or phone sessions after lockdown?
Barry: Yes, we also added an experience measure question about remote therapy and whether this format of therapy works for service users.
Sean: Ideally, we would have sent the service users the questionnaire to their home, so they have the time and privacy to complete it. But our service manager basically wanted an easier and quicker way of collecting right now. So at the end of their sessions via video or phone call, the clinician asked if the young person would like to take part in a survey and they read them out to the service user – so many young people are answering very positively in front of the clinician – so it’s hard to say how genuine these answers are. Another issue is for service users to differentiate between the session itself and the delivery of the session when being asked by the clinicians.
Barry: Interestingly, we are getting a high volume of returns. Service users are getting back to us. If the questionnaire would be sent to the service users’ homes though, the answers would be completely different than the answers they give directly over the phone. However, we would not get half of the questionnaires back if we would have sent paper versions to their homes. It is just the nature of this situation.
CORC: Thank you very much for your time and talking to us about your experience. Is there anything else CORC can help you with during this time?
Sean: With regards to further support I suppose it would be good to hear/know how other teams are coping with collecting data at this time and what other measures they are maybe utilising.
Are you using outcome measurement questionnaires as part of delivering your service remotely?
Visit our new guidance webpage, where we share advice and tips on working with feedback and outcome measures for services transitioning to working remotely with children, young people and families. We are reflecting on the research context, tackle legal issues like copyright and data protection and share practical tips and practical pointers for using questionnaires remotely.
We are also currently gathering responses from national and international CORC members, which we will collate and transfer onto an interactive map.
If you have any suggestions, tools, insights and experience that we can share in this area, then please email us at corc@annafreud.org or call us at +44 (0)20 7443 2225. We are happy to talk to you about what you are doing, the challenges or issues, and what you find works well. Other practitioners and services are keen to learn from you!